Christmas Bugs – Clostridium perfringens
What to do to avoid getting Clostridium perfringens this Christmas
December 22, 2017
Christmas is for eating! Eating large meals sharing with lots of people. These meals are not our usual day to day fare and if you’re not careful could lead to the case of a bad tummy bug, Clostridium perfringens – which could ruin all the holiday cheer for days or even weeks.
So, what to watch out for when preparing your feasts for your families this year?
Clostridium perfringens
A little-known bacterium called Clostridium perfringens can raise its scary head at Christmas time. Clostridium perfringens is a Gram-positive, rod-shaped, anaerobic, spore-forming pathogenic bacterium [1] . C. perfringens is the third most common cause of food poisoning in the United Kingdom though it can sometimes be ingested and cause no harm [2].
So how does it give us problems at Christmas time? Well it happily lives in the intestines of poultry (e.g. Turkey), which is a nice anaerobic (oxygen-free) environment and so comes into the house inside the large turkey purchased for Christmas dinner. C. perfringens is a member of the Clostridium species it is also a spore former which means it can withstand very high temperatures and so will be killed during cooking of the turkey – (even well-cooked turkeys so don’t blame the chef on this one!)
How it gets us, is how we handle the turkey after Christmas dinner is over…..
Here’s a scenario, everyone is full, and no one can be bothered cleaning up; let alone cut up the turkey and store the leftovers safely in the refrigerator. So instead the remains of the full carcass are left on the counter – cooling slowly in the lovely warm kitchen. No one even thinks about that turkey until late Christmas night when a nice cold turkey sandwich sounds appetising and this is where the danger lies. Clostridium perfringens multiply extremely fast in just 6.5 minutes under optimum conditions, within the short period of time of Christmas lunch to late night snack their levels can get dangerously high [3]. With no reheating one can ingest the toxin produced by these bacterium and symptoms typically abdominal cramping, diarrhoea, vomiting, and fever will ensue. The whole course usually resolves within 24 hours, but can last up to two weeks or even death in older or infirm people.
So how to avoid this disaster? Several things could have been done better.
- Cook your turkey following the instructions and make sure its internal temperature reaches 75C or above – eat whilst it’s still hot!
- Shortly after finishing the meal, make sure the turkey, stew or other large dish of leftovers is subdivided into smaller portions and stored in the refrigerator (Perfringens species do not do well at cold temperatures and won’t grow at all in the presence of oxygen)
- Reheat food which may have been subjected to slow cooling to piping hot – this will at least deactivate the toxin that C perfringens produce which is the actual culprit for making us sick
Follow those simple three rules and you and your family will avoid food poisoning from C perfringens, but beware there are two other pathogens closely linked to poultry – Salmonella and Campylobacter – for more information on those bad guys see our blogs ……
Examples of Clostridium perfringens outbreaks
| On May 7, 2010, “42 residents and 12 staff members at a Louisiana state psychiatric hospital were affected experienced vomiting, abdominal cramps, and diarrhea”. Three patients died within 24 hours. The outbreak was linked to chicken which was cooked a day prior to being served and was not cooled down according to hospital guidelines. The outbreak affected 31% of the residents of the hospital and 69% of the staff who ate the chicken. It is unknown how many of the affected residents ate the chicken. [5] |
| In January 2017, a restaurant in, New York was sued when 260 people were sickened after eating foods contaminated with Clostridium perfringens. “Officials from the Monroe County Department of Public Health closed down the Golden Ponds after more than a fourth of its Thanksgiving Day guests became ill. An inspection revealed a walk-in refrigerator with food spills and mould, a damaged gasket preventing the door from closing, and mildew growing inside.[6]: |
References
- https://en.wikipedia.org/wiki/Clostridium_perfringens
- Ryan, Kenneth J.; Ray, C. George (2004). Sherris Medical Microbiology: an Introduction to Infectious Diseases (4th ed.). New York: McGraw-Hill. p. 310. ISBN 0-8385-8529-9.
- The Essentials of Food Microbiology, p31, John Garbutt, pub Hodder Arnold 1997
- “Fatal Foodborne Clostridium perfringens Illness at a State Psychiatric Hospital — Louisiana, 2010″.Centers for Disease Control and Prevention. Retrieved 16 November 2013.
- “Mother, son sue eatery for Thanksgiving dinner food poisoning – Food Safety News”. 6 January 2017
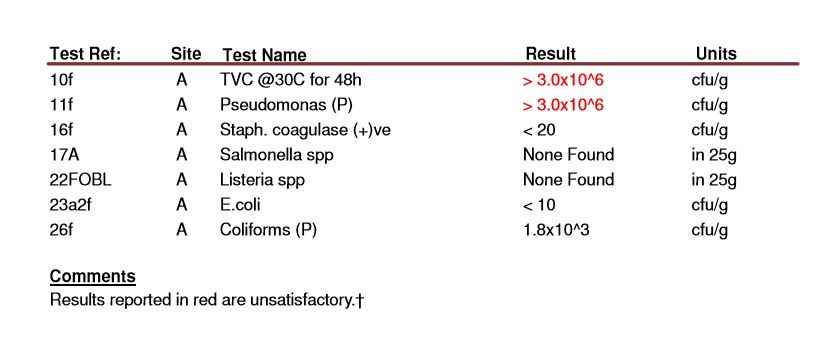
Express Micro Science conducts a range of microbiology food testing to help manufacturers identify bacteria in foods. We can test for a range of pathogenic and indicator organisms to look at specific bacteria and to help monitor factories. For more information please click on food testing to see the testing available from us, or please contact us directly.
Picture courtesy of: https://www.express.co.uk/life-style/health/889395/food-poisoning-symptoms-christmas-cook-turkey-bacteria